Cancer and Vitamin D
Did you know that Sunlight and Vitamin D deficiency is linked to Cancer


Studies had suggested that vitamin D played a key role in protecting against cancer, heart disease and diabetes - conditions that account for 60 to 70 per cent of all deaths in the West. Vitamin D is important because we are often short of it. Most healthy individuals get all the vitamins and minerals they need from eating a balanced diet, but vitamin D is the exception. It is made by the action of sunlight on the skin, which accounts for 90 per cent of the body's supply. Very little comes from food.
But the increasing use of sunscreens and the decreasing amount of time spent outdoors, especially by children, has contributed to what many scientists believe is an increasing problem of vitamin D deficiency. In the winter, the sun in Britain is barely strong enough to make the vitamin, and by spring, say scientists, 60 per cent of the population is deficient (defined as a blood level below 30ng per millilitre).
The traditional advice for avoiding these winter ailments has been to swallow large quantities of vitamin C. But we may have been turning to the wrong vitamin. Researchers from Winthrop University Hospital in Mineola, New York, found that giving supplements of vitamin D to a group of volunteers reduced episodes of infection with colds and flu by 70 per cent over three years. All the participants were Afro-Caribbean women whose dark skin means that they make less vitamin D. The researchers said that the vitamin stimulated "innate immunity" to viruses and bacteria. The decline in vitamin D levels between November and March could be the "seasonal stimulus" that accounts for the peak in colds and flu in the winter. "Since there is an epidemic of vitamin D insufficiency in the US, the public health implications of this observation could be great," the researchers wrote.
How to get it - and how much you should take
90 per cent of the body's supply of vitamin D is generated by the action of sunlight on the skin.
Vitamin D lasts for around 60 days in the body, so it needs regular topping up.
Twenty minutes twice a week in the sun with exposed hands, arms and face is adequate to maintain reserves.
There is no recommended supplementary dose in the UK.
In the US, the recommended supplementary dose is 400 international units a day.
Some scientists say that 1,000 international units of vitamin D a day may be necessary to prevent disease.
Vitamin D supplements cost around 5p a day.
Health benefits of the Sun: Vitamin D can reduce the risk of cancer by as much as 67%
Vitamin D is involved in the biology of all cells in your body, including your immune cells. A large number of studies have shown raising your vitamin D level can significantly reduce your risk of cancer.
Most recently, researchers found vitamin D and calcium supplementation lowered participants’ overall cancer risk by 30%.
Having a serum vitamin D level of at least 40 ng/ml reduces your risk for cancer by 67% compared to having a level of 20 ng/ml or less; most cancers occur in people with a vitamin D level between 10 and 40 ng/ml.
Vitamin D helps lower the risk of colorectal cancer by up to 58%, new study finds
New research involving over 1.3 million people shows that higher blood levels of vitamin D are linked to up to 58% lower risk of colorectal cancer, especially in women. Vitamin D helps slow cancer cell growth, support gut health and reduce inflammation, factors that are all important in preventing tumour formation in the colon.
A whopping 80% of adults are either deficient or insufficient in vitamin D, which significantly increases their risk of developing colorectal cancer over time. Getting regular sun exposure or supplementing with vitamin D has been shown to reduce the risk of polyps and tumours, even in people with a genetic risk for colon cancer.
Testing your vitamin D levels and correcting deficiencies through sunlight, supplements, or food is one of the most powerful and low-cost ways to reduce your colon cancer risk.
https://expose-news.com/2025/06/26/vitamin-d-helps-lower-risk-of-colorectal-cancer/
Higher Vitamin D Levels Lower Cancer Risk
This article was originally published on 10 April 2017.
Thousands of studies have been done on the health effects of vitamin D, and research shows it is involved in the biology of all cells and tissues in your body, including your immune cells. Your cells actually need the active form of vitamin D to gain access to the genetic blueprints stored inside.
This is one of the reasons why vitamin D has the ability to impact such a wide variety of health problems – from foetal development to cancer. Unfortunately, despite being easy and inexpensive to address, vitamin D deficiency is an epidemic around the world.
It’s been estimated that as many as 90% of pregnant mothers and newborns in the sunny Mediterranean region are even deficient in vitamin D,1 thanks to chronic Sun avoidance. A simple mathematical error may also deter many Americans and Canadians from optimising their vitamin D.
The Institute of Medicine (“IOM”) recommends a mere 600 IUs of vitamin D per day for adults. As pointed out in a 2014 paper, the IOM underestimates the need by a factor of 10 due to a mathematical error, which has never been corrected.
More recent research 4 suggests it would require 9,600 IUs of vitamin D per day to get a majority (97.5%) of the population to reach 40 nanograms per millilitre (ng/ml). The American Medical Association uses of 20 ng/ml as sufficient, but research shows 40 ng/mL should be the cutoff point for sufficiency in order to prevent a wide range of diseases, including cancer.
Research Again Concludes Vitamin D Lowers Cancer Risk
A large number of studies have shown raising your vitamin D level can significantly reduce your risk of cancer.
Most recently, a randomised clinical trial 5 by researchers at Creighton University, funded by the National Institutes of Health (“NIH”), found vitamin D and calcium supplementation lowered participants’ overall cancer risk by 30%.6,7,8
The study, which included more than 2,300 postmenopausal women from Nebraska who were followed for four years, looked at the effects of vitamin D supplementation on all types of cancer.
Participants were randomly assigned to receive either 2,000 IUs of vitamin D3 in combination with 1,500 mg of calcium, or a placebo for the duration of the study. Blood testing revealed that 25-hydroxyvitamin D (25(OH)D) levels were significantly lower in those who did develop cancer.
Joan Lappe, Ph.D., professor of nursing and associate dean of research at Creighton University’s College of Nursing, and lead author of the study, said:
The study provides evidence that higher concentrations of 25(OH)D in the blood, in the context of vitamin D3 and calcium supplementation, decrease risk of cancer … While people can make their own vitamin D3 when they are in the Sun near mid-day, sunscreen blocks most vitamin D production.
Also, due to more time spent indoors, many individuals lack adequate levels of vitamin D compounds in their blood. The results of this study lend credence to a call for more attention to the importance of vitamin D in human health and specifically in preventing cancer.
Full article can be found below:
https://expose-news.com/2023/12/28/health-benefits-of-the-sun/
More Evidence Showing Vitamin D Combats Cancer
Evidence continues to accumulate showing that vitamin D is a strong ally to combat cancer
Low vitamin D levels are linked to an increased risk of cancers, while vitamin D can attach to the vitamin D receptor (VDR) in your cells, setting off a series of signals that may affect how they grow, develop and survive
Although increasing vitamin D levels may help to reduce cancer deaths, health officials rarely recommend optimizing levels for this purpose
Vitamin D targets cancer in multiple ways, including anticancer, antimetastatic and anti-tumorigenic effects
The best way to optimize your vitamin D level is via regular sun exposure, which enhances production of melatonin — a potent anticancer agent
I strongly recommend getting sensible sun exposure each day, and one of the reasons why is because it helps naturally optimize your vitamin D levels. Low vitamin D levels are linked to an increased risk of cancers,1 while vitamin D can attach to the vitamin D receptor (VDR) in your cells, setting off a series of signals that may affect how they grow, develop and survive.2
In this way, vitamin D acts like a brake on the process of cell growth in many tissues of the body, helping to control the speed at which cells multiply. This is particularly important when it comes to cancer because one of the key features of this disease is cells growing out of control. Moreover, vitamin D has been observed in animal studies to help delay some age-related changes by activating another important pathway via the vitamin D receptor.
This pathway involves a molecule called Nrf2, which plays a crucial role in protecting your body from oxidative stress and DNA damage — two factors that are commonly linked to the development of cancer.3 Overall, evidence continues to accumulate showing that vitamin D is a strong ally to combat cancer.
Vitamin D Reduces Cancer Mortality
Worldwide, cancer is the no. 2 cause of death, behind only cardiovascular disease.5 Meanwhile, the global prevalence of vitamin D deficiency (defined as a level of less than 20 ng/mL) and insufficiency (defined as a level of 20 to less than 30 ng/mL) is 40% to 100%.6 Although increasing vitamin D levels may help to reduce cancer deaths, health officials rarely recommend optimizing levels for this purpose.
For example, research has shown that once you reach a minimum serum vitamin D level of 40 ng/mL, your risk for cancer diminishes by 67%, compared to having a level of 20 ng/mL or less.7
A 2023 systematic review and meta-analysis published in Ageing Research Reviews also found vitamin D3 supplementation reduced cancer mortality by 6%. This wasn’t considered statistically significant, but when only studies involving daily vitamin D intake were analyzed, cancer mortality dropped by a significant 12%.8 According to the researchers:9
“From a biological perspective, it is plausible that a sufficient vitamin D status has an impact on cancer prognosis: by binding to the vitamin D receptor (VDR), the active hormone 1,25-dihydroxyvitamin D (1,25(OH)2D) influences signaling pathways that regulate cell proliferation, differentiation, and cell survival, and thus acts as an anti-proliferative agent in many tissues and can slow the growth of malignant cells.”
Other research also supports vitamin D’s role in protecting against cancer death. In one study of 25,871 patients, vitamin D supplementation was found to reduce the risk for metastatic cancer and death by 17%. The risk was reduced by as much as 38% among those who also maintained a healthy weight.10,11
What’s particularly noteworthy is this study only gave participants 2,000 IU of vitamin D daily and didn’t measure their blood levels. Despite these research flaws, a significant benefit was still found. However, other research has found even more striking benefits, including a GrassrootsHealth analysis published in PLOS ONE.
It showed women with a vitamin D level at or above 60 ng/mL (150 nmol/L) had an 82% lower risk of breast cancer compared to those with levels below 20 ng/mL (50 nmol/L).12 Meanwhile, risks of lung cancer, colorectal cancer, breast cancer, bladder cancer and lymphoma are higher in people with low vitamin D levels, while having higher levels is associated with a better prognosis in cases of breast and colorectal cancers.13
The Ageing Research Reviews study further revealed that daily vitamin D supplementation was particularly beneficial for people aged 70 and over, as well as those who took vitamin D daily and were later diagnosed with cancer. Study author Ben Schöttker, Ph.D., with the German Cancer Research Center in Heidelberg, further explained:14
“This does imply that basically everyone aged 50 and older, including people who have never had cancer, might profit from vitamin D supplementation if they are vitamin D insufficient … Doctors cannot know who might develop cancer at a later time.”
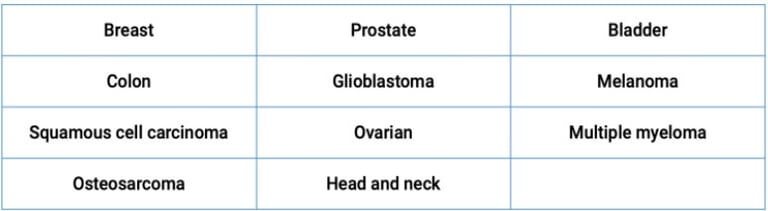
Vitamin D Has Anticancer Effects Against Many Types of Cancer
A mini review on the impact of vitamin D on cancer, published in The Journal of Steroid Biochemistry and Molecular Biology, pointed out that while vitamin D is widely recognized for its essential role in regulating the balance of minerals in the body, a deficiency has been linked to the onset and progression of various cancers.15 Vitamin D targets cancer in multiple ways, including:16
Vitamin D and Cancer: A Quick Review and a Look at New Research
Anticancer effects, which means it targets different stages of cancer development and progression, including the initiation, growth and spread of cancer cells.
Antimetastatic effects, which refers to the ability to stop cancer cells from spreading from the original tumor site to other parts of the body. Since metastasis is often responsible for the fatal outcomes of cancers, preventing the spread can significantly improve survival rates.
Anti-tumorigenic, meaning vitamin D helps prevent tumor formation or the growth of tumors. This can involve mechanisms like inducing cell death in cancer cells, blocking cell cycle progression, or inhibiting pathways that fuel tumor growth.
The review highlighted vitamin D’s role against the following cancers
In terms of breast cancer, the leading cause of death for women globally, vitamin D deficiency is common among patients, and those who are deficient are more likely to have more aggressive and harder-to-treat subtypes of breast cancer, such as higher grade and estrogen receptor-negative tumors.
The study also highlighted the role of genetic differences in the VDR that could influence breast cancer risk. In particular, in certain populations like North Indian women from New Delhi, variations in the VDR gene were identified as potential risk factors.18
In prostate cancer — the most common cancer in men — low levels of vitamin D were linked to high levels of dihydrotestosterone (DHT) in the prostate which is associated with the progression of prostate cancer.19 In addition, vitamin D may influence the activity of sirtuin 1 (SIRT1), which is known as a longevity protein. Optimizing your vitamin D levels may help boost your body’s natural cancer defenses, in part, via mechanisms involving SIRT1.20
Additional research suggests there may be considerable variation in how different individuals’ genes respond to vitamin D supplementation, which might explain why not everyone benefits equally from extra vitamin D.
For best results, the scientists suggest vitamin D supplementation should be personalized and “advocate for options tailored to individual vitamin D needs, combined with a comprehensive intervention that favors prevention through a healthy environment and responsible health behaviors.”21
Why Sun Exposure Is the Best Source of Vitamin D
On a typical sunny day, your body may produce up to 25,000 international units (IU) of vitamin D,22although many people aren’t in the sun enough to optimize their vitamin D levels. However, I strongly recommend getting your vitamin D from proper sun exposure, if possible, as it provides benefits beyond vitamin D optimization.
Higher levels of vitamin D may even serve as a marker for healthy sun exposure, which in turn may be responsible for many of the health benefits, which include reduced risk of cancer and increased longevity, attributed to vitamin D. Regular sun exposure, for instance, enhances production of melatonin — a potent anticancer agent.23
Near-infrared rays from the sun penetrate deep into your body and activate cytochrome c oxidase, which in turn stimulates the production of melatonin inside your mitochondria. Your mitochondria produce ATP, the energy currency of your body. A byproduct of this ATP production is reactive oxidative species (ROS), which are responsible for oxidative stress.
Excessive amounts of ROS will damage the mitochondria, contributing to suboptimal health, inflammation and chronic health conditions such as diabetes, obesity and thrombosis (blood clots). But melatonin essentially mops up ROS that damage your mitochondria. So, by getting plenty of sun exposure during the day, your mitochondria will be bathed in melatonin, thereby reducing oxidative stress.24,25
If you’re unable to get adequate sun exposure each day, vitamin D supplementation may be necessary. Keep in mind that 20 ng/mL, which is often used as the cutoff for vitamin D deficiency, has repeatedly been shown to be grossly insufficient for good health and disease prevention, which means the true prevalence of people without optimal levels of vitamin D is even greater.
The only way to determine how much sun exposure is enough and/or how much vitamin D3 you need to take is to measure your vitamin D level, ideally twice a year. Once you’ve confirmed your vitamin D levels via testing, adjust your sun exposure and/or vitamin D3 supplementation accordingly. Then, remember to retest in three to four months to make sure you’ve reached your target level.
The Optimal Vitamin D Level for Cancer Prevention
The optimal level for health and disease prevention, including cancer prevention, is between 60 ng/mL and 80 ng/mL (150-200 nmol/L), while the cutoff for sufficiency appears to be around 40 ng/mL. In Europe, the measurements you’re looking for are 150 to 200 nmol/L and 100 nmol/L respectively.
It’s important to remember that calcium, vitamin D3, magnesium and vitamin K2 must be properly balanced for optimal overall health. Your best and safest bet is to simply eat more calcium-, magnesium- and vitamin K2-rich foods, along with sensible sun exposure.
However, if you find supplementation is necessary after a serum vitamin D test, also supplement with magnesium and vitamin K2 (MK-7) to ensure proper balance. You’ll also want to ensure you’re following an overall healthy lifestyle to reduce your cancer risk as much as possible. As researchers explained in Nutrients:26
“Vitamin D supplementation is not the magic pill that miraculously solves the cancer burden or that can replace a healthy lifestyle. It is necessary to foster a good environment and invigorate a healthy lifestyle, including a high-quality diet and physical activity. Both have been proven to confer health benefits in many diseases, including cancer, and are the best preventive measures available.”
Vitamin D and Cancer: A Quick Review and a Look at New Research
Low circulating vitamin D levels are associated with an increased risk of cancers
2023 July, Seraphin et al – The impact of vitamin D on cancer: A mini review
“Vitamin D deficiency has been linked to the development and progression of a number of cancer types.”
Vitamin D continues to show positive anti-cancer effects against many types of cancer.
Demographic studies recommend vitamin D supplementation to prevent cancer.
In general, the normal range for circulating 25(OH)D is 30–50 ng/mL
deficiency is defined as < 20 ng/mL
https://www.globalresearch.ca/vitamin-d-and-cancer-a-quick-review-and-a-look-at-new-research/5855101?utm_campaign=magnet&utm_source=article_page&utm_medium=related_articles
Vitamin D and breast cancer risk
A connection between vitamin D level and the risk of developing breast cancer has been implicated for a long time, but its clinical relevance had not yet been proven. Sascha Abbas and colleagues from the working group headed by Dr. Jenny Chang-Claude at the German Cancer Research Center (Deutsches Krebsforschungszentrum, DKFZ), collaborating with researchers of the University Hospitals in Hamburg-Eppendorf, have now obtained clear results: While previous studies had concentrated chiefly on nutritional vitamin D, the researchers have now investigated the complete vitamin D status. To this end, they studied 25-hydroxyvitamin D (25(OH)D) as a marker for both endogenous vitamin D and vitamin D from food intake
The result of the study involving 1,394 breast cancer patients and an equal number of healthy women after menopause was surprisingly clear: Women with a very low blood level of 25(OH)D have a considerably increased breast cancer risk. The effect was found to be strongest in women who were not taking hormones for relief of menopausal symptoms. However, the authors note that, in this retrospective study, diagnosis-related factors such as chemotherapy or lack of sunlight after prolonged hospital stays might have contributed to low vitamin levels of breast cancer patients.
In addition, the investigators focused on the vitamin D receptor. The gene of this receptor is found in several variants known as polymorphisms. The research team of the DKFZ and Eppendorf Hospitals investigated the effect of four of these polymorphisms on the risk of developing breast cancer. They found out that carriers of the Taql polymorphism have a slightly increased risk of breast tumors that carry receptors for the female sex hormone estrogen on their surface. No effects on the overall breast cancer risk were found. A possible explanation offered by the authors is that vitamin D can exert its cancer-preventing effect by counteracting the growth-promoting effect of estrogens.
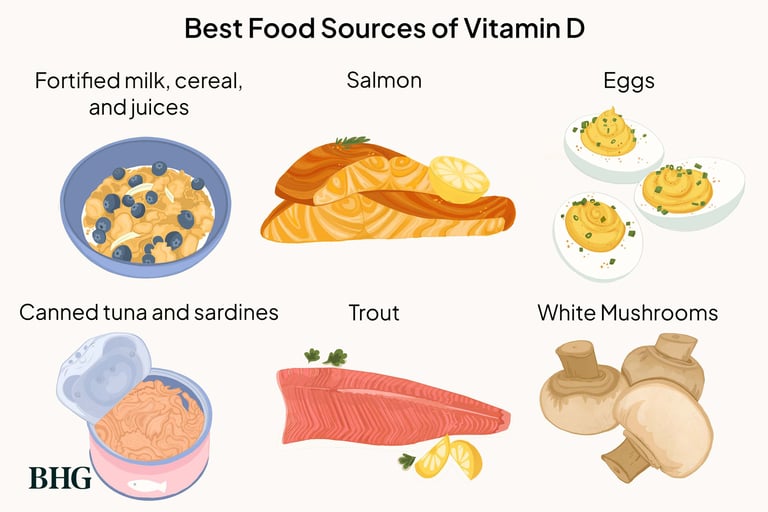
Besides its cancer-preventing influence with effects on cell growth, cell differentiation and programmed cell death (apoptosis), vitamin D regulates, above all, the calcium metabolism in our body. Foods that are particularly rich in vitamin D include seafish (cod liver oil), eggs and dairy products. However, the largest portion of vitamin D is produced by our own body with the aid of sunlight.
https://www.sott.net/article/154106-Vitamin-D-and-breast-cancer-risk
Dermatology's Disastrous War Against The Sun
The forgotten side of skin health and the necessity of sunlight
•Skin cancers are by far the most commonly diagnosed cancer in the United States, so to prevent them, the public is constantly told to avoid the sun. However, while the relatively benign skin cancers are caused by sun exposure, the ones responsible for most skin cancer deaths are due to a lack of sunlight.
•This is unfortunate because sunlight is arguably the most important nutrient for the human body, as avoiding it doubles one’s rate of dying and significantly increases their risk of cancer.
•A strong case can be made that this dynamic was a result of the dermatology profession (with the help of a top PR firm) rebranding themselves to skin cancer fighters, something which allowed them to become one of the highest paying medical specialities in existence. Unfortunately, despite the billions that is put into fighting it each year, there has been no substantial change in the number of skin cancer deaths.
•In the article below, it discusses the dangers of the conventional skin cancer treatments, the most effective ways for treating and preventing skin cancer, and some of the best strategies for having a healthy and nourishing relationship with the sun.
https://www.midwesterndoctor.com/p/dermatologys-disastrous-war-against?utm_source=profile&utm_medium=reader2
Sunlight naturally boosts our immune systems
Sensible sun exposure has many health benefits. Many are the result of vitamin D production, which occurs when your skin is exposed to UV light, but many others are unrelated to vitamin D.
Research shows both blue light and UVA light boost the activity of T lymphocytes. As little as five to 10 minutes of sun exposure was needed to boost immune cell activity.
The healthiest blue light is from the sun, as it is balanced by near-infrared radiation, which activates cytochrome C oxidase in your mitochondria and helps optimise ATP production.
Mounting research confirms that sun avoidance may be at the heart of a large number of health problems. Not only does your body produce vitamin D in response to sun exposure on bare skin, but sunlight also produces several other health benefits that are unrelated to vitamin D production.
In fact, humans appear to have a lot in common with plants in this regard – we both need direct sun exposure to optimally thrive, and while artificial lighting sources offering specific light spectrums may be helpful for various problems, ideally we need the full spectrum of light that natural sunlight offers.
More recently, researchers at Georgetown University Medical Centre (“GUMC”) published a laboratory study using cells in Petri dishes, showing that exposure to blue and ultraviolet (“UV”) light increases T cell activity – white blood cells involved in immune function and fighting infections
https://expose-news.com/2024/01/28/sunlight-naturally-boosts-our-immune-systems/
Top 25 Vitamin D Rich Fruits and Vegetables
https://www.felixhospital.com/blogs/top-25-vitamin-d-rich-fruits-and-vegetables